Fill in Your Tb Test Form
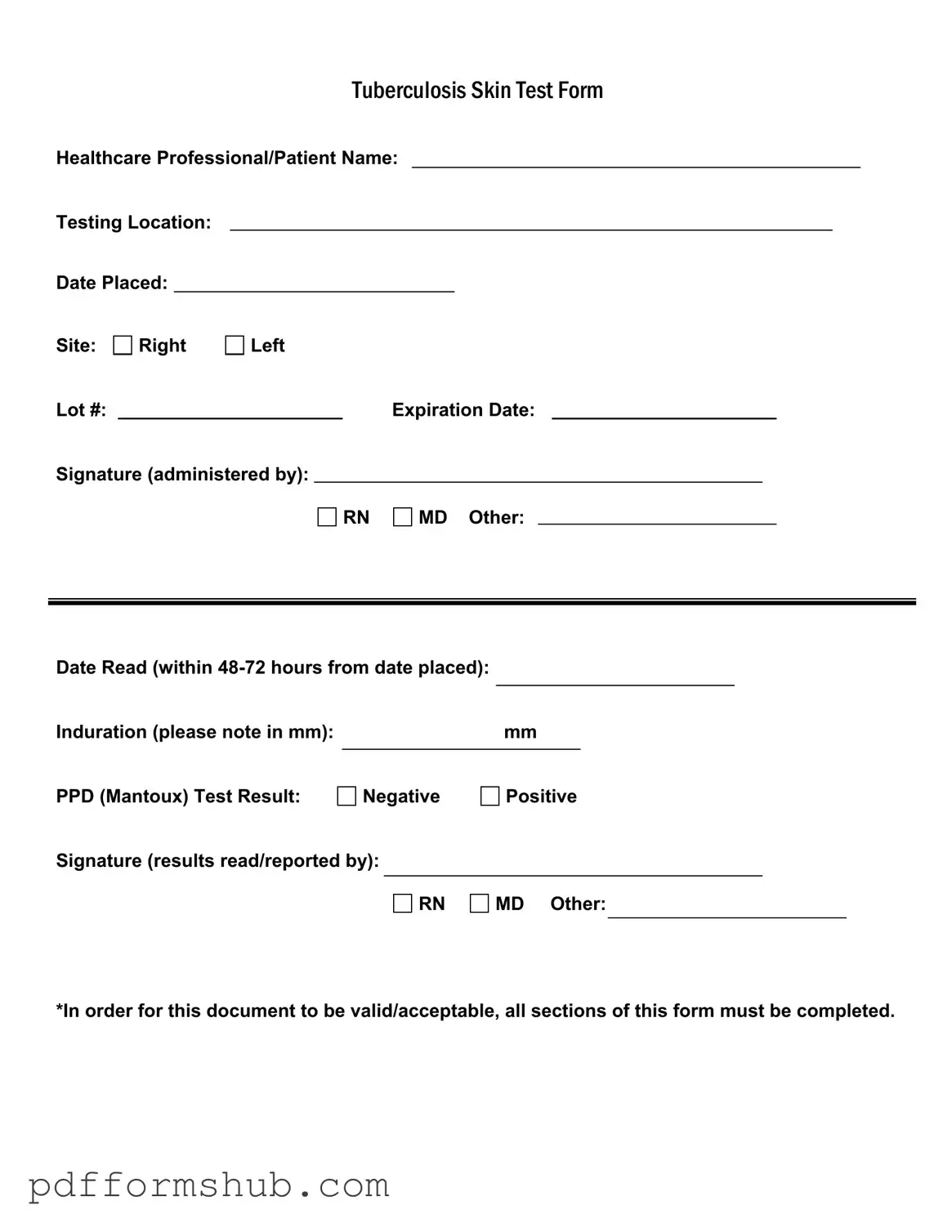
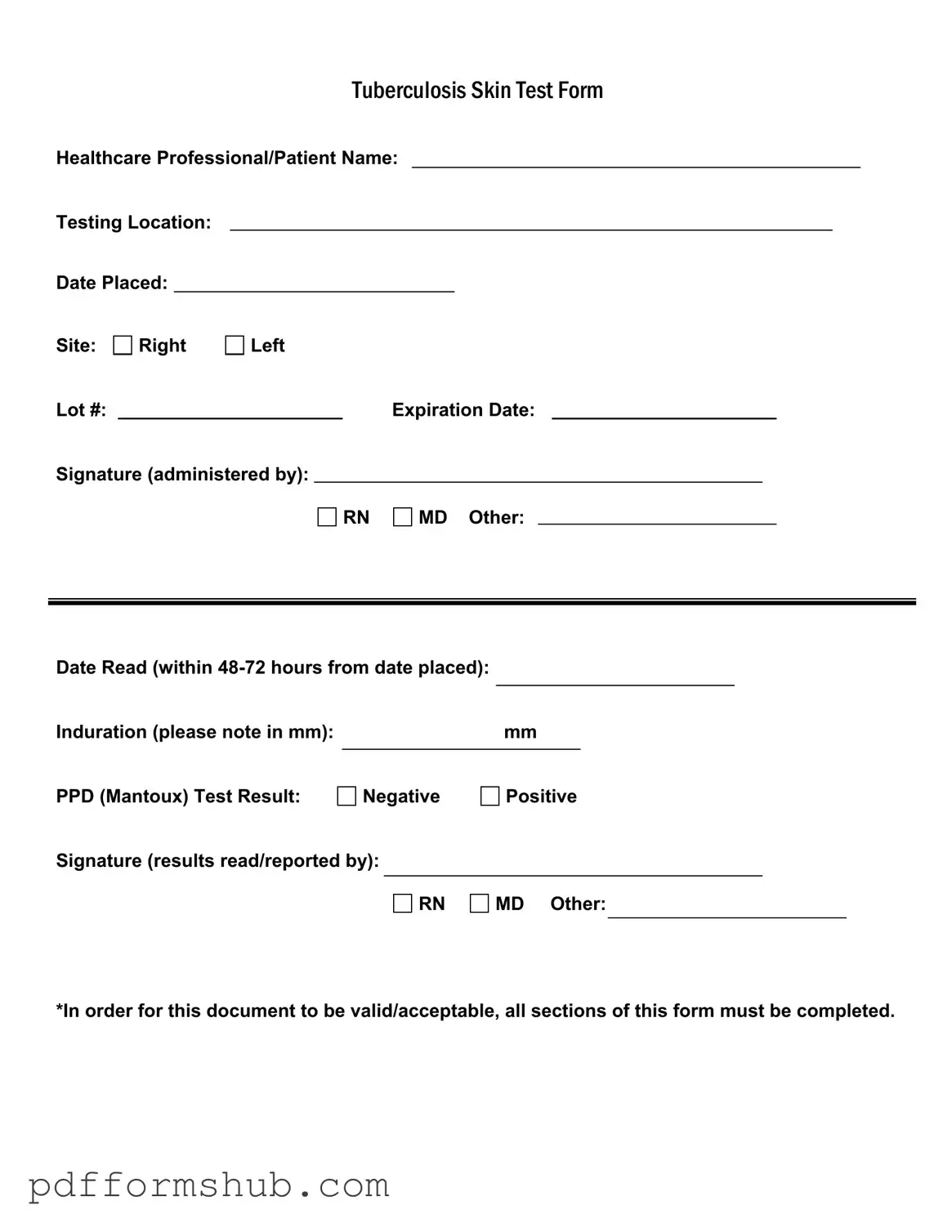
The Tuberculosis Skin Test Form is a document used to record essential information about a tuberculosis skin test, including patient details and test results. This form is crucial for healthcare professionals to ensure accurate testing and reporting. To complete your tuberculosis screening, fill out the form by clicking the button below.
Customize Form
Fill in Your Tb Test Form
Customize Form
Customize Form
or
Free PDF Form
Short deadline? Complete this form now
Complete Tb Test online without printing hassles.