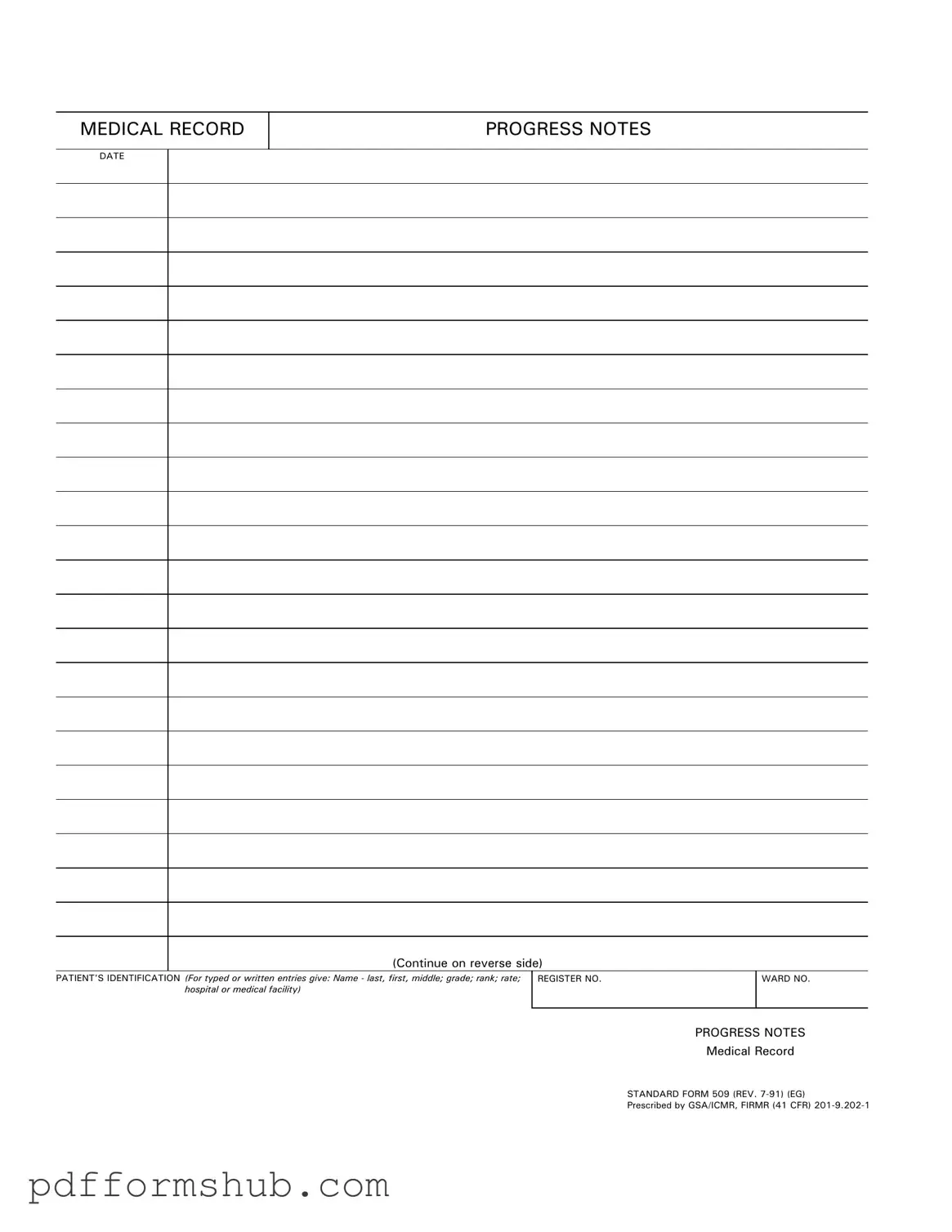
Fill in Your Progress Notes Form
The Progress Notes form is a crucial document used in medical settings to track a patient's ongoing treatment and progress. This form includes essential information such as the patient's identification, date, and specific notes related to their care. To ensure accurate and effective communication within the healthcare team, it is important to fill out this form correctly; click the button below to get started.
Customize Form
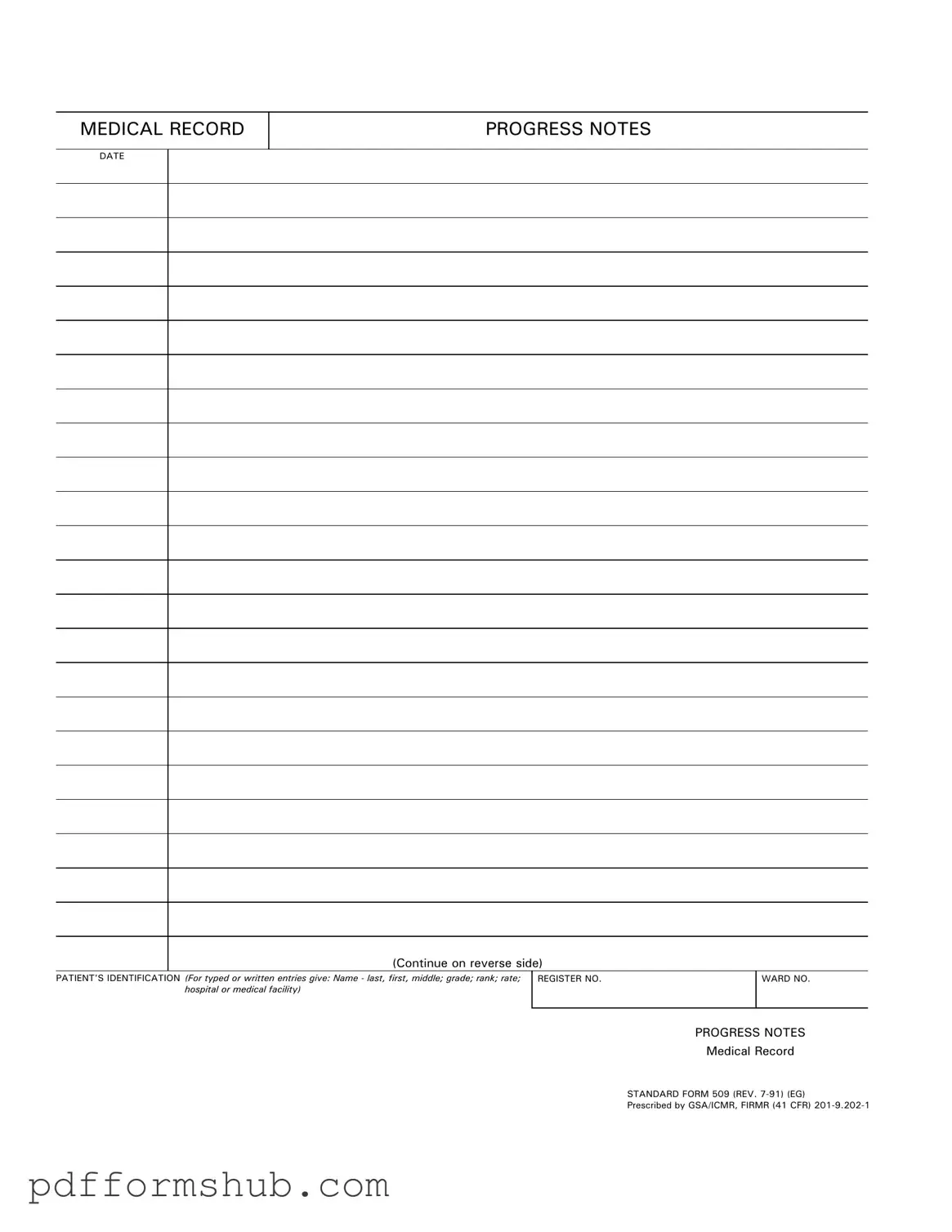
Fill in Your Progress Notes Form
Customize Form
Customize Form
or
Free PDF Form
Short deadline? Complete this form now
Complete Progress Notes online without printing hassles.