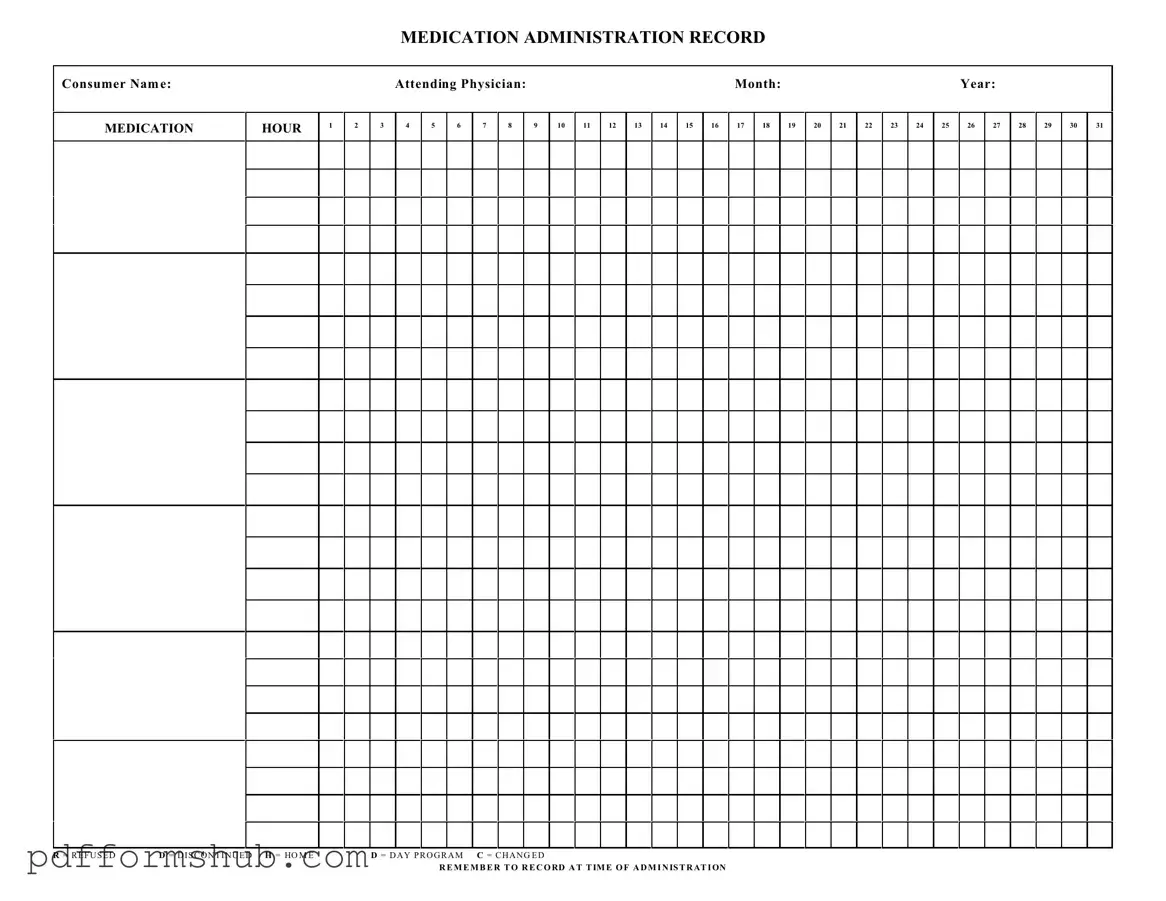
Fill in Your Medication Administration Record Sheet Form
The Medication Administration Record Sheet is a crucial tool used to document the administration of medications to patients. This form ensures that all medications are given accurately and helps healthcare providers track any changes or refusals. By maintaining clear records, healthcare professionals can provide better care and ensure patient safety.
Start filling out the form by clicking the button below.
Customize Form
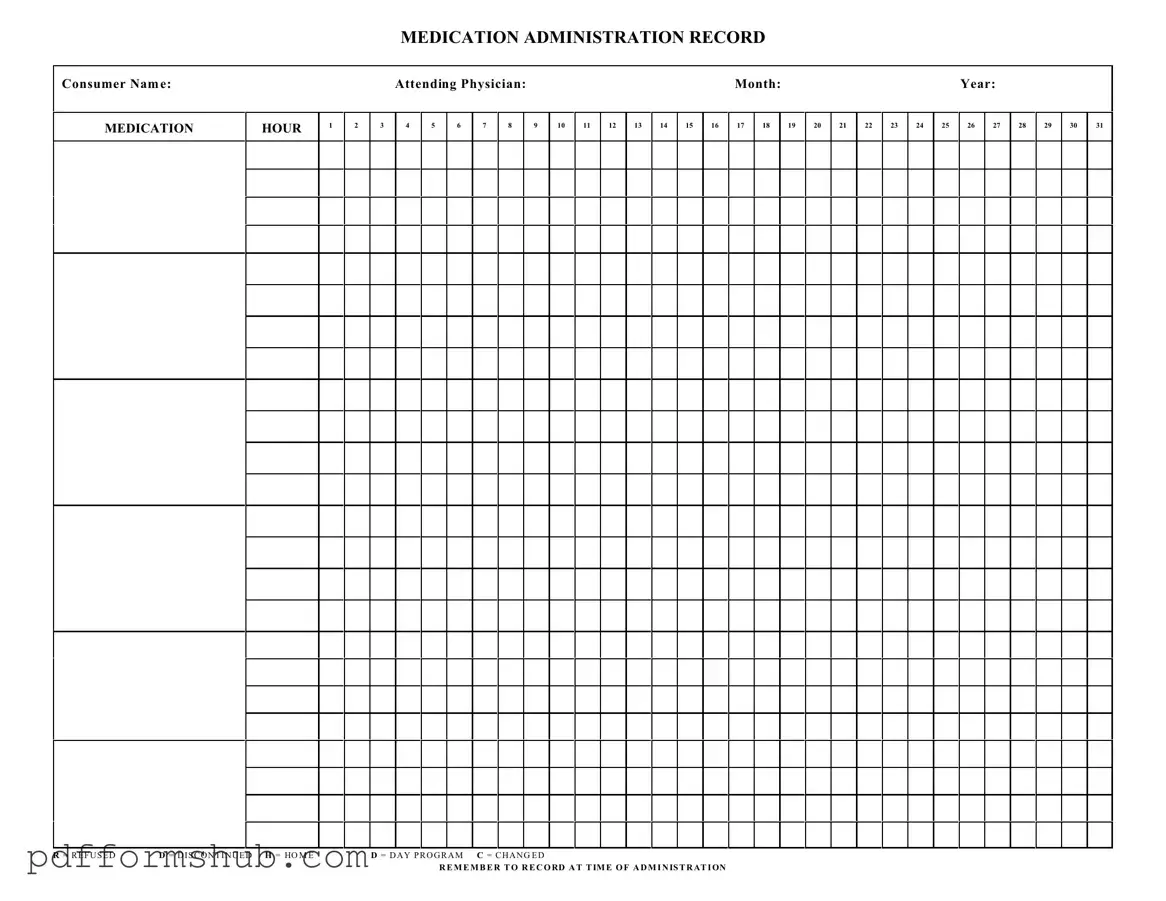
Fill in Your Medication Administration Record Sheet Form
Customize Form
Customize Form
or
Free PDF Form
Short deadline? Complete this form now
Complete Medication Administration Record Sheet online without printing hassles.