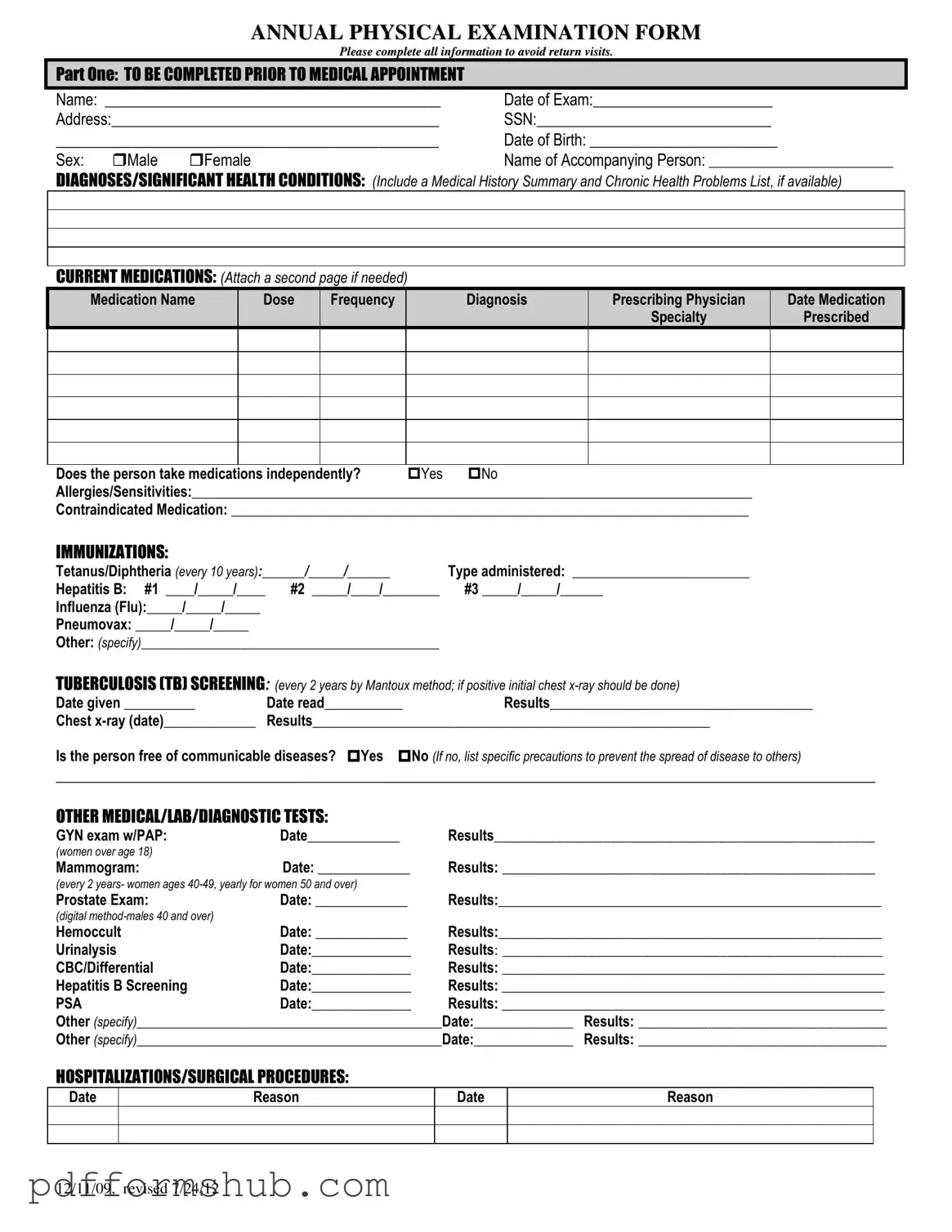
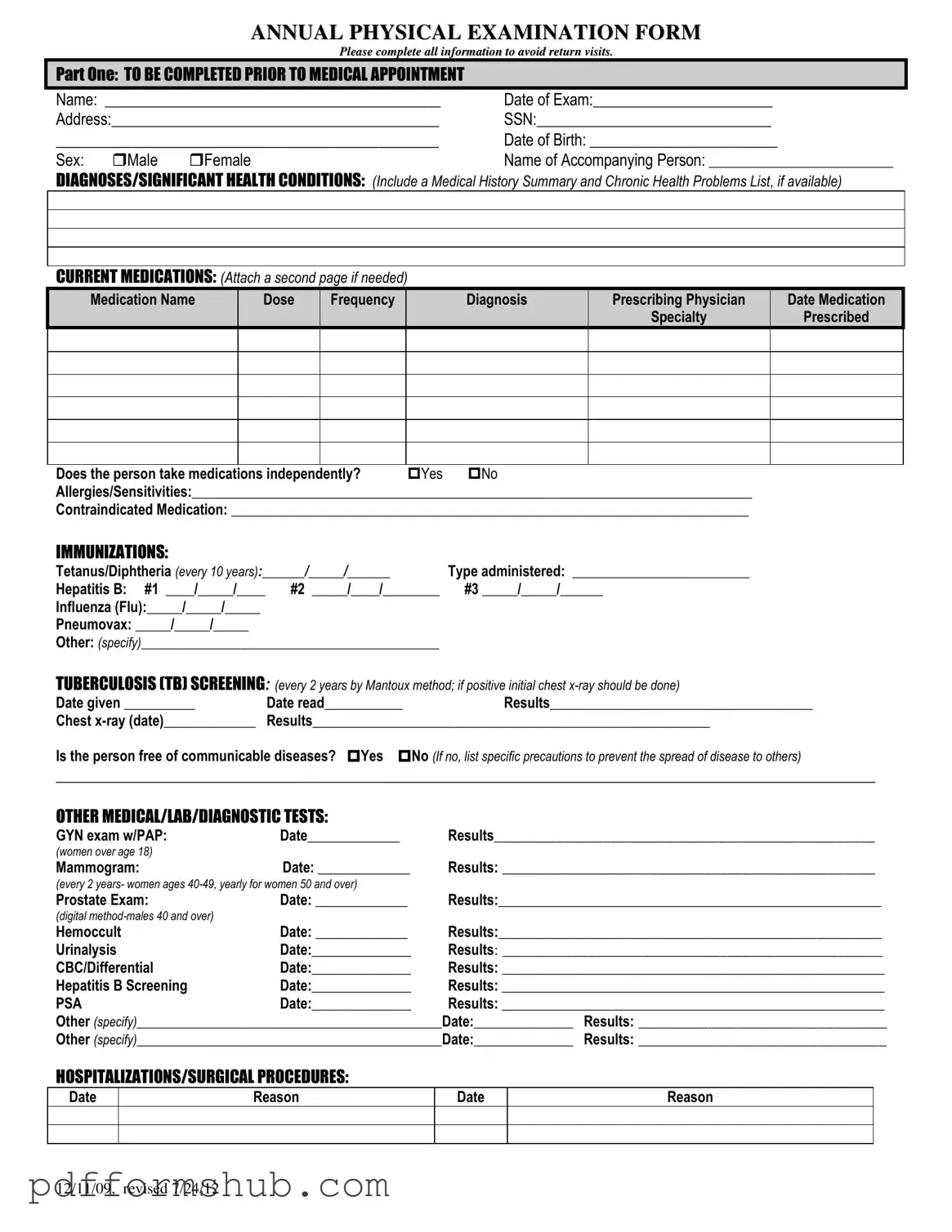
Fill in Your Annual Physical Examination Form
The Annual Physical Examination Form is a crucial document used to gather essential health information before a medical appointment. It ensures that healthcare providers have all necessary details, including medical history, current medications, and any significant health conditions. Completing this form accurately helps streamline the examination process and reduces the need for return visits.
Fill out the form by clicking the button below.
Customize Form
Fill in Your Annual Physical Examination Form
Customize Form
Customize Form
or
Free PDF Form
Short deadline? Complete this form now
Complete Annual Physical Examination online without printing hassles.