Fill in Your Advance Beneficiary Notice of Non-coverage Form
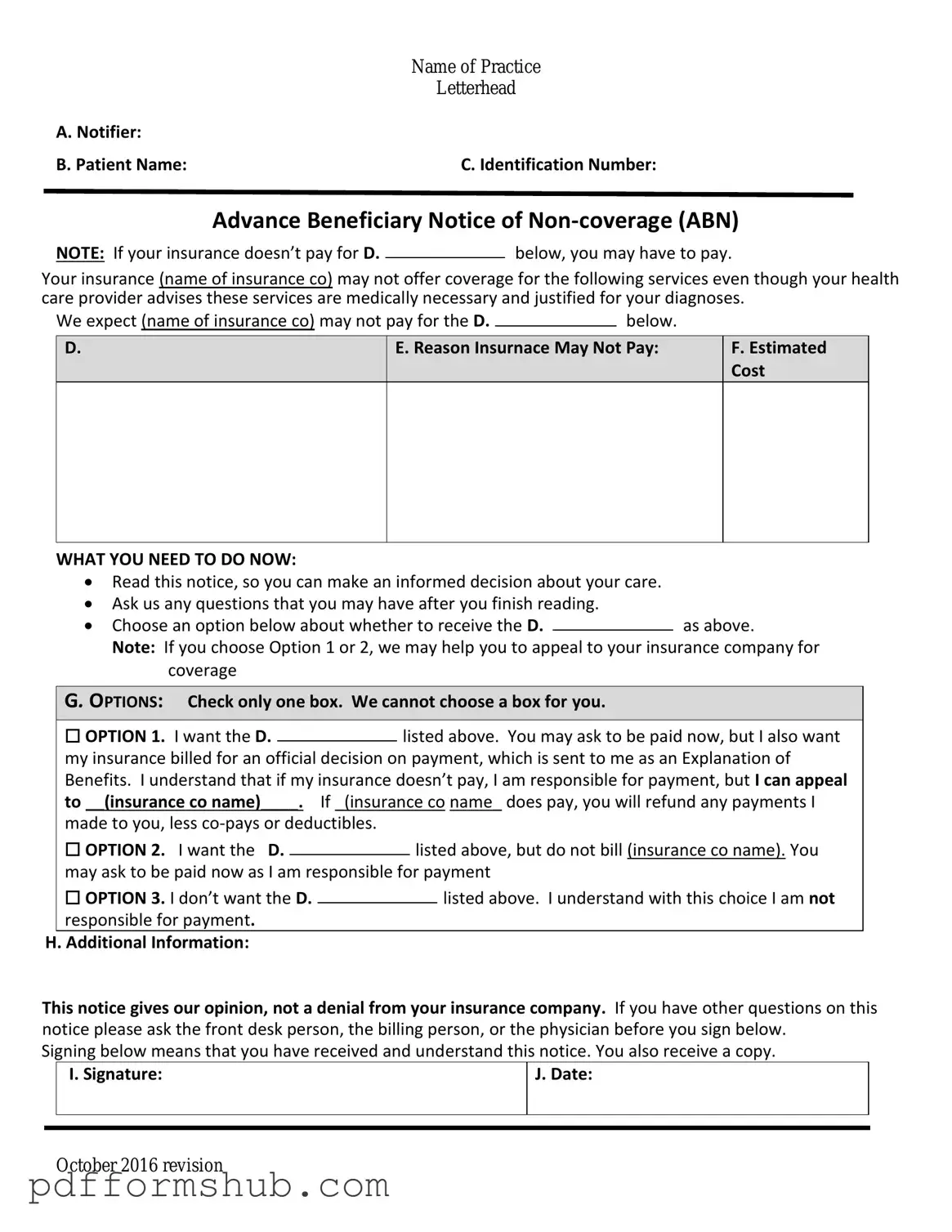
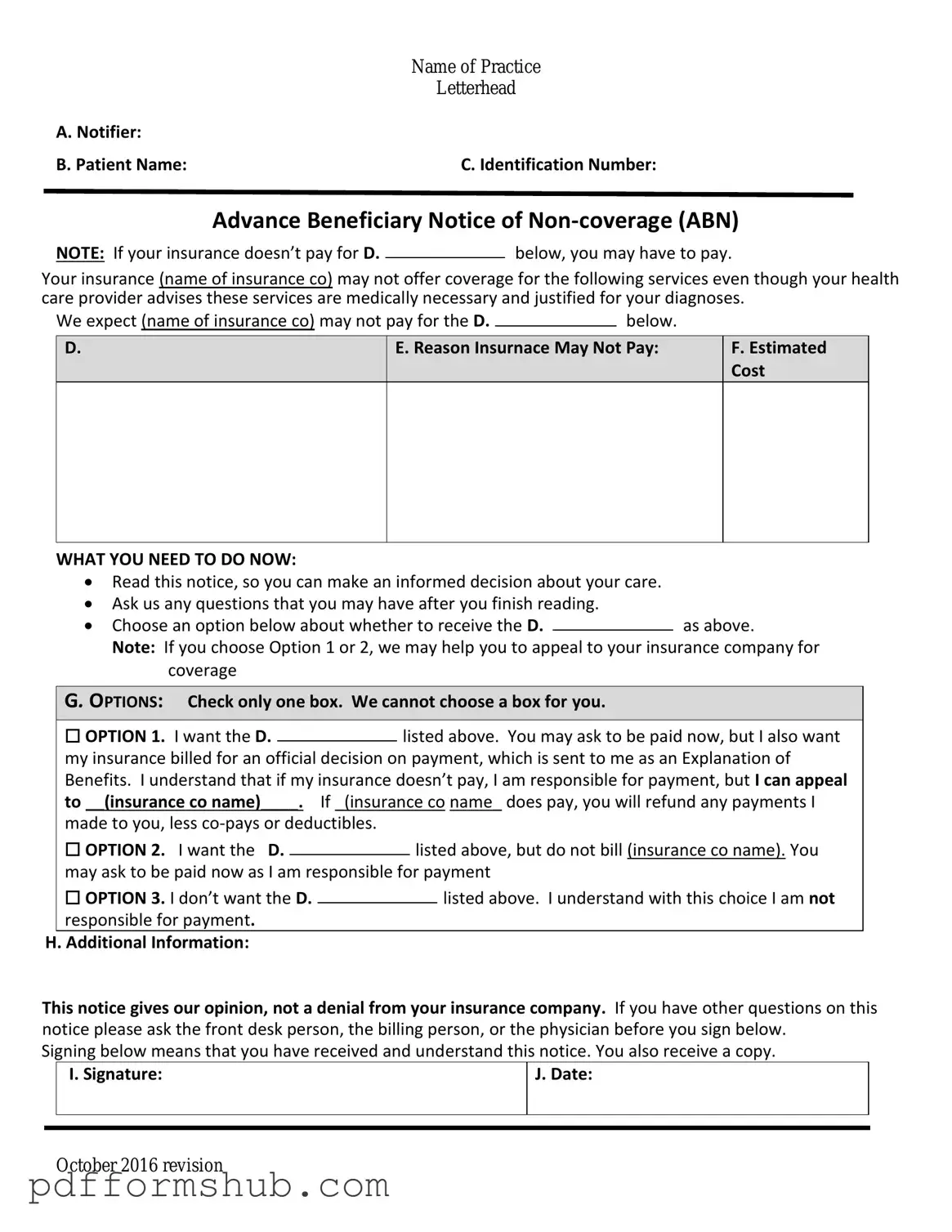
The Advance Beneficiary Notice of Non-coverage (ABN) is a crucial document used in the Medicare system to inform beneficiaries that a service may not be covered by Medicare. This form empowers patients by providing them with the information needed to make informed decisions about their healthcare costs. Understanding the ABN can help you avoid unexpected bills, so be sure to fill out the form by clicking the button below.
Customize Form
Fill in Your Advance Beneficiary Notice of Non-coverage Form
Customize Form
Customize Form
or
Free PDF Form
Short deadline? Complete this form now
Complete Advance Beneficiary Notice of Non-coverage online without printing hassles.